credits: wscs.com
– following up on my previous post (more than six years ago!) –
Anthony Atala is a pediatric surgeon, urologist and directs the Wake Forest Institute for Regenerative Medicine (WFIRM) in North Carolina. Together with 400 colleagues and in a work that spans more than three decades, he has successfully implanted in human patients a variety of tissues regenerated from the patient’s own cells. Dr. Atala talked to 3DPrint.com about ways to translate the science of regenerative medicine into clinical therapy and the importance of adopting new technologies, as well as some of the challenges.
“Back in the 90’s we created by hand, even without using the printer, bladders, skin, cartilage, urethra, muscle and vaginal organs, and later implanted them successfully in patients. The printer automated what we were already doing and scaled it up making some of the processes easier. Still, the technology has its own challenges. With hand made constructs you have more control as you are creating the tissue, but with the printed structure everything has to be built in before it is created, so that you have to have the whole plan and information ready to go once you push that ‘start’ button”.

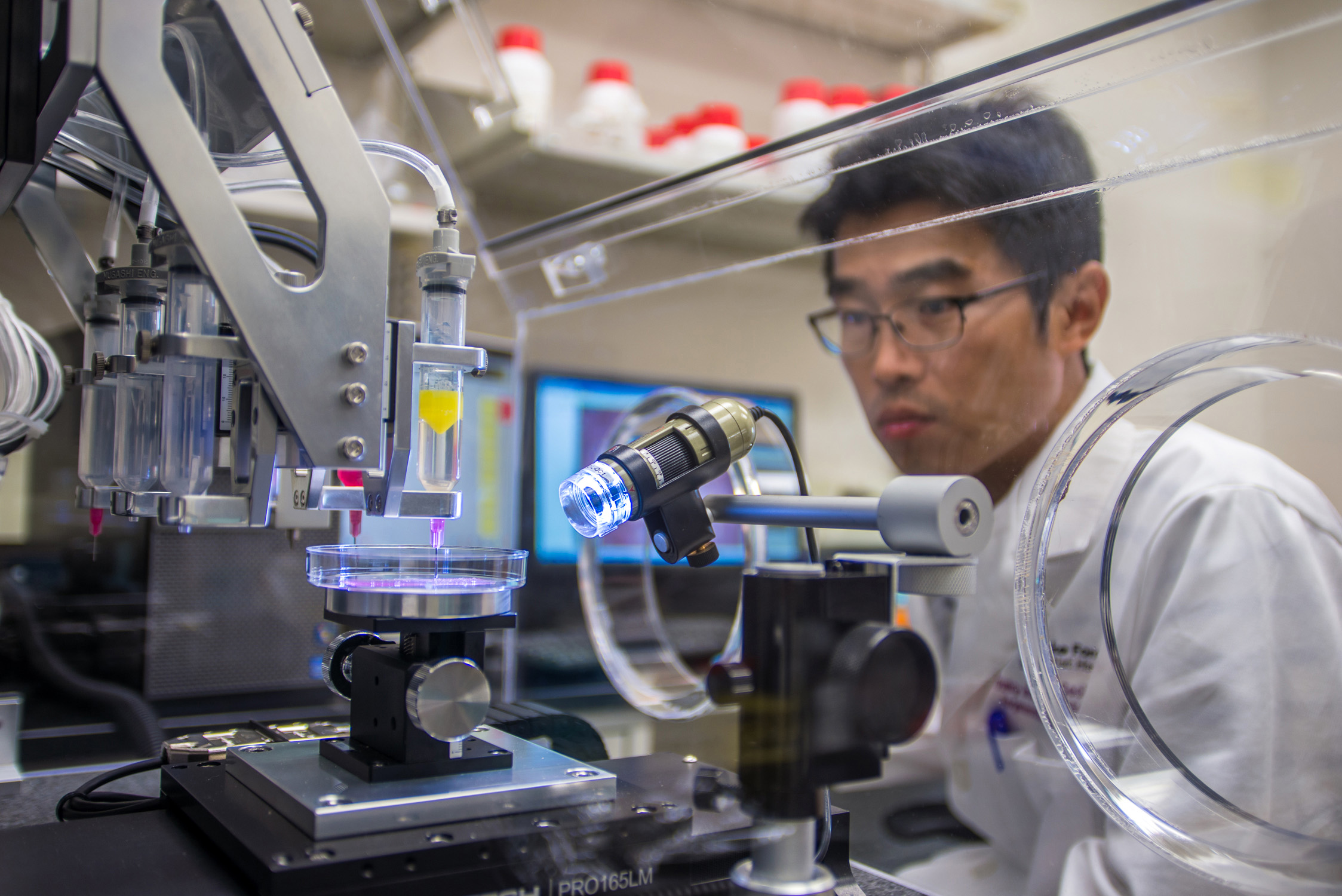
The WFIRM is working to grow tissues and organs and develop healing cell therapies for more than 40 different areas of the body, from kidney and trachea to cartilage and skin. Dr. Atala and his team of scientists have been first in the world to implant lab-grown tissues and organs into patients. Starting in 1990 with most of their research and implanting the first structures at the end of that decade, using a 3D printer to build a synthetic scaffold of a human bladder, which they then coated with cells taken from their patients. New research at WFIRM shows innovative wound healing through the use of a bedside 3D skin printer.

“Today, we continue to develop replacement tissues and organs, and are also working to speed up the availability of these treatments to patients. The ultimate goal is to create tissues for patients. Part of that is taking a very small piece of the patients tissue from the organ that we are trying to reconstruct, like muscle or blood vessels, only to expand the cells outside of the body and then use them to create the organ or structure along with a scaffold or a hydrogel which is the glue that holds the cells together. We have been doing this for quite some time with patients and 16 years ago we realized that we needed to scale up the technology and automate it to work with thousands of patients at a time, so we started thinking about 3D printers, and began using the typical desktop inkjet printer which was modified in-house to print cells into a 3D shape”.

The living cells were placed in the wells of the ink cartridge and the printer was programmed to print them in a certain order. The printer is now part of the permanent collection of the National Museum of Health and Medicine. According to Dr. Atala, all the printers at the WFIRM continue to be built in-house specifically to create tissues, so that they are highly specialized and able to create cells without damaging the tissue as it gets printed. Inside the institute, more than 400 scientists in the fields of biomedical and chemical engineering, cell and molecular biology, biochemistry, pharmacology, physiology, materials science, nanotechnology, genomics, proteomics, surgery and medicine work to try to develop some of the most advanced functional organs for their patients. At WFRIM they are focusing on personalized medicine, whereby the scientists use the sample tissue from the patient they are treating, grow it and implant it back to avoid rejection. Dr. Atala claims that “these technologies get tested extensively before they are implanted into a patient”, and that “it could take years or even decades of research and investigation before going from the experimental phase to the actual trial in humans. Our goal for the coming decade is to keep implanting tissues in patients, however, the most important thing for us is that we temper peoples expectations because these tissues come out very slowly and they come out one at a time, so we don’t give false hopes and provide the technology to patients who really need them. Working with over 40 different tissues and organs, means that about 10 applications of this technologies are already in patients. The research we have done helps us categorize tissues under order of complexity, so we know that flat structures (like skin) are the least complex; tubular structures (such as blood vessels) have the second level of complexity, and hollow non-tubular organs, including the bladder or stomach, have the third level of complexity because the architecture of the cells are manifold. Finally, the most complex organs are solid ones, like the heart, the liver and kidneys, which require more cells per centimeter”.
