Awesome people always pop their knuckles when they are with someone who clearly state they can’t stand it. The cracking sound that our knuckles (but also our fingers themselves, and sometimes our elbows and knees) produce when we “stretch” them is somehow addictive. I thought it would be interesting to understand what makes our joints pop in this strange way and I asked God Google for that.
First of all we have to focus on Diarthrodial Joints, better known (maybe) as Synovial Joints. We have synovial joints all over our body: in our hands, wrists, arms, but also in our shoulders and knees. Wikipedia actually says that a synovial joint is “the most common and most movable type of joint in the body of a mammal”.
As probably said in  some previous post, in this kind of articulation two bones get in contact with each other through cartilage surfaces. A Joint Capsule acts as a connective tissue that folds the whole articulation and keeps everything at the right place, ensuring mobility and stability at the same time. This capsule is filled by Synovial Fluid, which has two main functions:
some previous post, in this kind of articulation two bones get in contact with each other through cartilage surfaces. A Joint Capsule acts as a connective tissue that folds the whole articulation and keeps everything at the right place, ensuring mobility and stability at the same time. This capsule is filled by Synovial Fluid, which has two main functions:
- it continuously lubricates the articulation;
- it is a source of nutrients for the cells that maintain the joint cartilage.
The synovial fluid contains dissolved gases, mainly oxygen (O2), nitrogen (N2) and carbon dioxide (CO2). These gases are responsible for the popping sound we are trying to explain! After this necessary introduction (yep, I’ve just spoiled the name of the murderer), let’s come back to the action of cracking our knuckles.

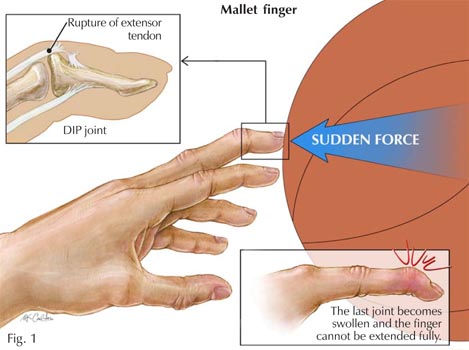
 In order to pop our knuckles, we can stretch or bend our fingers. In any case, the bones of each knuckle joint (which is a synovial joint) pull apart. As we can easily figure out, by doing this the knuckle joint capsule gets stretched.
In order to pop our knuckles, we can stretch or bend our fingers. In any case, the bones of each knuckle joint (which is a synovial joint) pull apart. As we can easily figure out, by doing this the knuckle joint capsule gets stretched.
 This causes the volume of the joint capsule to increase a bit (+ 15-20%). This slight change of volume is followed by a corresponding decrease of the synovial fluid pressure. As a consequence, the gases in the fluid suddenly become less soluble and they form small bubbles inside the tiny joint capsule. The process of “rapid pressure change -> formation of small cavities in the liquid -> formation of bubbles that immediately implode” is defined by fluid dynamics as cavitation.
This causes the volume of the joint capsule to increase a bit (+ 15-20%). This slight change of volume is followed by a corresponding decrease of the synovial fluid pressure. As a consequence, the gases in the fluid suddenly become less soluble and they form small bubbles inside the tiny joint capsule. The process of “rapid pressure change -> formation of small cavities in the liquid -> formation of bubbles that immediately implode” is defined by fluid dynamics as cavitation.
The implosion of such small bubbles is thought to be the origin of the cracking sound that we hear while popping our knuckles. It normally takes 20-30 minutes for the gas to properly redissolve into the synovial fluid and reestablish the initial conditions. This means that after more or less half an hour of silence we’ll be able to start having fun again 🙂
Many people seem to be frightened by the idea that excessive knuckle popping may lead to unpleasant consequences, such as arthritis or sudden death (…). Luckily, a few studies confirm that apparently there is no correlation between knuckle cracking and osteoarthritis in the finger joints.  Another study, however, showed that pathological addiction to knuckle popping may affect the joint capsule soft tissue (higher risk of damages and wear) and worsen hand grip strength conditions. On the positive side, there’s evidence of slightly increased mobility in joints right after popping (mainly thanks to muscle relaxation induced by this action).
Another study, however, showed that pathological addiction to knuckle popping may affect the joint capsule soft tissue (higher risk of damages and wear) and worsen hand grip strength conditions. On the positive side, there’s evidence of slightly increased mobility in joints right after popping (mainly thanks to muscle relaxation induced by this action).
In conclusion, we can crack our knuckles whenever we want, but we’d better do it in moderation.
sources: this website, this other one and wikipedia